By Carmel Shachar, Sean McBride, and Shannon MacDonald
Via The Boston Globe
Imagine being told while sitting in your car in a strip mall parking lot that you have a brain tumor, hoping your spotty cellphone service is strong enough to make out what your physician is saying. Imagine telling your doctor embarrassing symptoms of an illness while sitting in a crowded coffee shop. Imagine your child getting sick on a long-planned vacation, only to be told you must travel back to your home state if you want to speak to your longtime pediatrician.
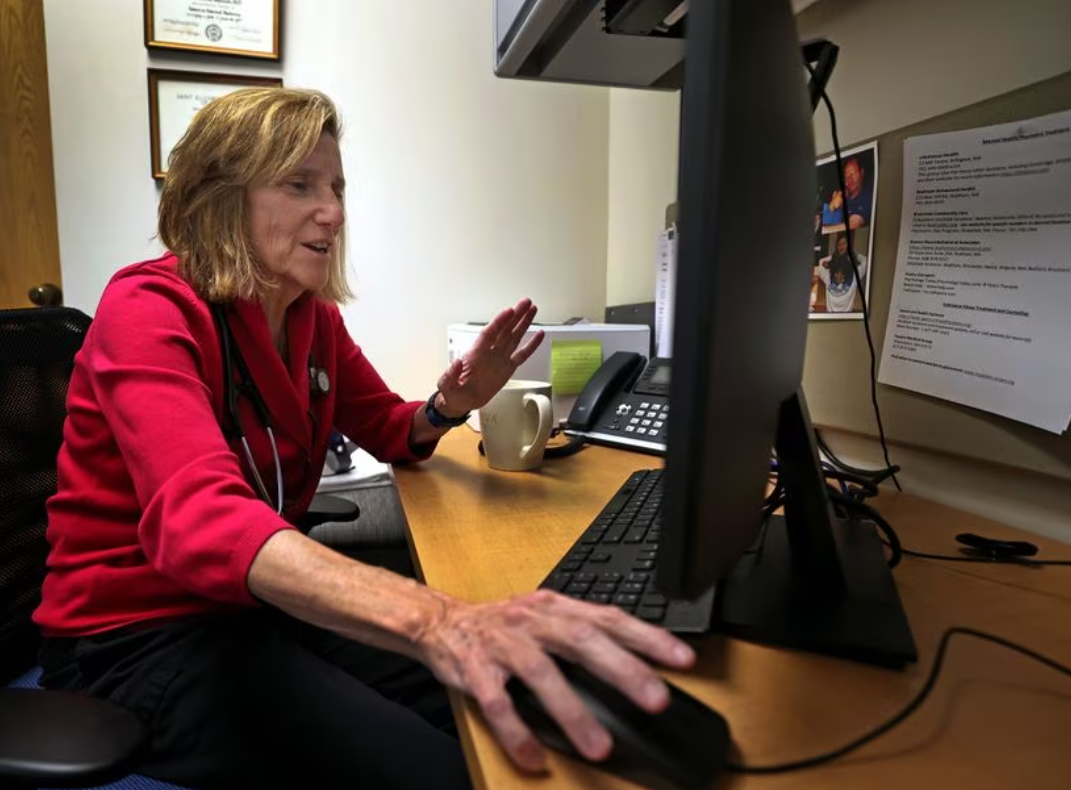
Unfortunately these scenarios are becoming increasingly common due to outdated physician licensure laws. Most states require a physician to be licensed in the state where the patient is physically located if they want to practice medicine, make a diagnosis, or provide treatment for them. Before the digital revolution in health care, this was rarely an issue because the patient was almost always in the same room as their doctor. Now it’s common to have the patient in one state and their physician in another and care is over Zoom or on the phone.
To comply with licensure laws, physicians must ask patients to be in the same state. Patients have to drive across a state border and sit in a parking lot to attend a telehealth visit. The United States’ outmoded licensure system also means that some patients are not able to utilize telehealth at all, instead having to travel long distances to see the appropriate out-of-state specialist in person.
The pandemic created a telehealth boom. While we will likely never go back to the peak pandemic levels of telehealth, our national experiment with it has proven that telehealth can provide quality care while reducing costs to patients and society more broadly. Both patients and physicians report satisfaction with telehealth encounters, including patients saying they would prefer for some of their visits to remain virtual and physicians reporting no perceived adverse outcomes from telemedicine.
This telehealth boom was facilitated by a thoughtful and necessary regulatory response from federal and state governments during the COVID-19 pandemic, lifting restrictions on telehealth, including often waiving in-state licensure requirements. Unfortunately, with the end of the Federal COVID-19 Public Health Emergency on May 11, that regulatory window is fast closing. Many states have already ended their pandemic telehealth waivers, once again requiring physicians to be fully licensed in the state their patient “sits.”
This requirement creates a burden for patients and their families, especially those who need specialist care such as cancer patients or children with rare medical conditions. Depending on where they live, these patients often find the right specialists out of reach because they cannot afford travel expenses but licensing requirements block telehealth visits. This puts some of our most miraculous, cutting-edge treatment out of reach for too many Americans.
Despite efforts to help physicians with interstate practices through the Interstate Medical Licensure Compact, getting licensed in multiple states is an administrative gantlet. Physicians looking to practice in multiple states have to be fingerprinted again and again, sit through multiple, superfluous tests, and juggle inconsequential differences in medical education requirements. Getting licensed in all 50 states would cost about $90,000 per physician, excluding biannual renewal fees. It is inefficient and to many cost-prohibitive to ask physicians to chase licenses in every state so that they can better help their patients.
With the September end–date of the federal public health emergency fast approaching, the nation’s physician licensure system must be updated to better support patients by facilitating interstate telehealth visits. One approach would be for each state to establish several exceptions to their licensure requirements. The Federation of State Medical Boards has already articulated some useful exceptions, such as episodic follow-up care when the patient is temporarily in a different state (for example, getting sick while on vacation or a college student returning home for school breaks) and follow-up after travel for surgical or medical treatments. These exceptions would certainly help to minimize travel for some patients, but they would still leave many patients feeling abandoned and without access to care.
A better alternative would be for medical licenses to work the way drivers’ licenses work. Because of the Driver License Compact, drivers do not need to collect multiple licenses to do cross-country trips. The federal government could set some standards for state-issued telemedicine licenses, similar to its standard-setting role in establishing the REAL ID program. This approach would minimize compliance burdens on physicians, allowing them to focus on patient care instead of licensure complexities.
Patients should not have to sit in parking lots or coffee shops or fly across the country to have important telehealth appointments. Access to specialists should not be limited to those fortunate enough to live near world-class medical centers or those with the financial means to constantly travel to medical hubs such as Boston or New York. During the pandemic, state and federal governments fixed these challenges, but that regulatory grace is fast evaporating. State-by-state licensing system is no longer a source for improved care quality, but rather an anti-competitive regulatory thicket that drives up prices and decreases access for patients. It is vital that the federal government act quickly to allow physicians to provide telehealth across state borders and end parking lot medicine.
Carmel Shachar is executive director of the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics and incoming assistant clinical professor of law at Harvard Law School. Dr. Sean McBride is incoming president of the medical staff and a radiation oncologist at Memorial Sloan Kettering Cancer Center. Dr. Shannon MacDonald is an associate radiation oncologist at Mass General Brigham and an associate professor of radiation oncology at Harvard Medical School.
Filed in: Op-Ed
Tags: Carmel Shachar, Center for Health Law and Policy Innovation, Health Law and Policy Clinic
Contact Office of Clinical and Pro Bono Programs
Website:
hls.harvard.edu/clinics
Email:
clinical@law.harvard.edu