Via MV Times
By: Brittany Bowker
If nutritious food prevents chronic disease and promotes long-term health, why shouldn’t it be included in our healthcare plans? That’s the notion behind Food Is Medicine, a Massachusetts coalition dedicated to increasing access to vital nutrition services for every community in the commonwealth.
The coalition, which stems from a team at the Center for Health Law and Policy Innovation at Harvard Law School, launched June 18, and aims to connect food and nutrition with health and wellness, as well as legislative policy. On Monday, representatives from Food Is Medicine met Island stakeholders at the Martha’s Vineyard Hospital (MVH) to discuss goals, ideas, and initiatives.
“Food and nutrition are at the cornerstone of health and wellness,” said hospital CEO Denise Schepici to a group of about 30 gathered over lunch in the hospital’s community room. Representatives from Island Grown Initiative (IGI), the hospital, Island Health Care (IHC), Family Planning, Social Services, Elder Services, and the Island Food Pantry, among other invested community members, attended.
According to a study from the Greater Boston Food Bank and Children’s HealthWatch, food insecurity costs the state $1.9 billion in annual healthcare costs.
“The cost of the healthcare system increases as severity of food insecurity increases,” said Sarah Downer, primary author of the Food Is Medicine state plan. “If someone is in the hospital and they’re malnourished, it’s going to be more expensive to the system … We want to explore what role the healthcare system plays when it interacts with the food system.”
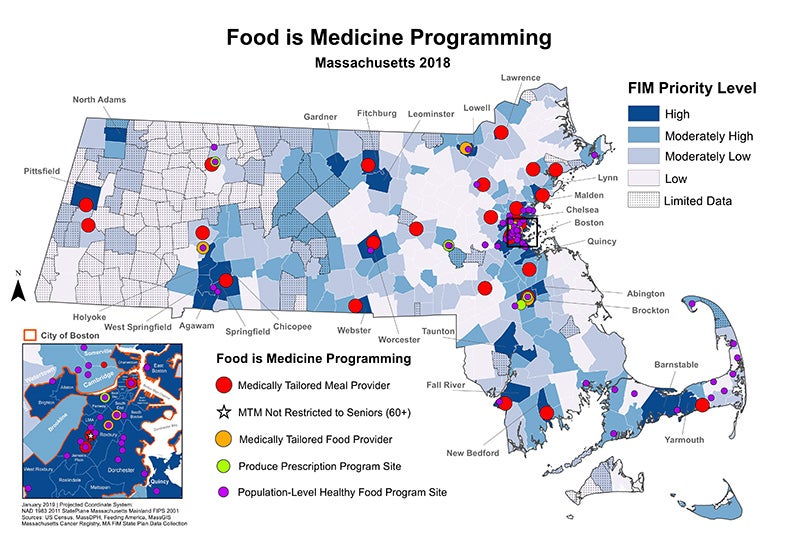
The Food Is Medicine coalition came up with four intervention initiatives:
- Medically tailored meals designed by a registered dietitian to respond to a specific medical condition.
- Medically tailored groceries, a package of nonprepared grocery items selected by a registered dietitian as part of a treatment program. The recipient is usually capable of picking up the food and preparing it at home.
- Produce prescription/voucher programs for free or discounted produce distributed by healthcare providers to address a specific health condition. Redeemable at retail grocery stores, farmers markets, or CSA (community-supported agriculture) programs.
- Population-level healthy food programs, where antihunger programs partner with healthcare providers to distribute healthy food to any patient regardless of health status.
The hospital and IHC, along with health providers across Massachusetts, have begun adopting these initiatives. The hospital has rolled out two food insecurity primary-care screening questionnaires developed by Hunger VitalSign and Children’s HealthWatch to identify young children and families who may need assistance, with inquiries like these:
- Within the past 12 months, we worried whether our food would run out before we got money to buy more.
- Within the past 12 months, the food we bought just didn’t last, and we didn’t have money to buy more.
“People are more frank when asked to answer a questionnaire,” said Aletheia Donahue, primary-care physician at MVH. “It’s an effective, validated screening tool where we can get data and compare it with other institutions.”
IHC is rolling out a similar screening questionnaire for all social determinants of health, according to Kathleen Samways, chief quality officer at IHC. “We know we have something really big to tackle,” Samways said.
Just this week, IHC launched a produce prescription pilot in partnership with IGI. Six chosen patients will receive free locally grown produce and free cooking classes.
“We’ll start getting a sense for the way these programs can influence blood pressure, weight, and shopping habits,” said Noli Taylor, community food education director at IGI.
“Patient profiles show the need is huge,” said IHC nurse practitioner Marcia Denine.
Food Is Medicine is also focused on getting food access resources ingrained in statewide healthcare systems. “We want to make sure healthcare providers are equipped with all the information they need to screen a patient for food insecurity,” Downers said. “It would be ingrained in the system. There would always be something in the community for the patient to be referred to.”
Taylor gave an overview of the existing food-equity services on Martha’s Vineyard. Among them are the Food Equity Network, a group of over 22 organizations focused on tackling food equity issues on the Island. There’s the Island Food Pantry, which doubled its number of clients between 2017 and 2018, and is seeing a 30 to 80 percent monthly increase in 2019, according to Island Food Pantry executive director Kayte Morris. The Island also has robust SNAP, WIC, and HIPservices. According to Taylor, more than 600 Islanders utilize SNAP, which represents a fraction of individuals who could sign up for those services. “More outreach and coordination are necessary, and I’m looking forward to being a part of that,” said Eve Gates of Dukes County Social Services.
The Island clergy are another robust food and grocery voucher distributor. Mandi Moran of the Good Shepherd Parish said they distributed 75,000 pounds of food in one year. There’s a food resource hotline, 508-693-7900, ext. 410, launched by Martha’s Vineyard Community Services in partnership with IGI. IGI’s gleaning program has collected and redistributed 25,000 pounds of produce from local farms, and 1,000 pounds of produce from grocery stores. IGI also has a processed-food program, and a partnership with Kitchen Porch Catering to prepare and freeze food to make it easier for Islanders to eat. IGI is expanding its processing program with Camp Jabberwocky this winter. IGI also offers a free lunch program, and a year-round Mobile Market.
“Even though so many of us are working on this, we know we’re not reaching everyone,” Taylor said. “We’re excited to be working with the hospital and health center. Together we can have a stronger food-equity support structure, and our programs will be more impactful.”
“The hospital is committed to being a ‘Food Is Medicine’ leader,” Donahue added.
Food Is Medicine is working closely with state policy and legislation. “We’re in the business of making sure we’re on the agenda,” Downer said. Sen. Julian Cyr, D-Truro, was supposed to appear at Monday’s gathering, but had a prior engagement. Cyr, who represents the Island in the state Senate, has been instrumental in getting Food Is Medicine through to policymakers, according to Downer. “In the healthcare legal and policy world, it’s hard to get people to pay attention until you have studies,” Downer said. “We now have bodies of emerging research showing things we’ve been witnessing.”
“This is all very heartening to me,” IGI executive director Rebecca Haag concluded. “The only way we start making a difference is if we collaborate and cooperate — just sharing information. Let’s get back together in a year and see how far we’ve come.”
Filed in: In the News
Contact Office of Clinical and Pro Bono Programs
Website:
hls.harvard.edu/clinics
Email:
clinical@law.harvard.edu