A collaboration between Harvard University researchers and the National Commission on Correctional Health Care has yielded the first detailed survey on the effects of the coronavirus pandemic on correctional facilities in the United States.
The ongoing survey has so far collected data from more than 320 facilities housing approximately 10 percent of the country’s inmates across 47 states. While not necessarily representative of all correctional institutions, the results nonetheless are vital for policymakers responding to the pandemic in their own states and communities.
Among the key findings:
- Correctional officers, like the general population, are at risk for contracting of COVID-19 infection, with a higher infection rate than inmates.
- Many protocols call for screening inmates and staff for COVID-19 on a regular basis, but a significant fraction of facilities still lack access to lab testing.
- The nationwide shortage of PPE as well as ancillary supplies (such as cleaning products and thermometer probes) is also a problem for correctional health care operations.
The survey was devised as a collaboration between Professor Marcella Alsan, MD, MPH, PhD, from Harvard Kennedy School, Professor Crystal Yang, JD, PHD, from Harvard Law School, and the National Commission on Correctional Health Care. NCCHC sent the initial survey and a daily follow-up questionnaire to jails, prisons, and juvenile detention facilities nationwide. Results are providing unique insights into the prevalence of the novel coronavirus and the associated COVID-19 disease among the incarcerated population as well as the challenges correctional health staff are facing as they respond to the pandemic.
“By definition, jails and prisons are closed environments and therefore potential hotspots for virus spread,” said Deborah Ross, NCCHC chief executive officer. “As corrections grapples with the challenges of the pandemic, this study provides very important data in an area that is often overlooked.”
Read a Q&A with professors Yang and Alsan: Assessing the effect of the COVID-19 pandemic on correctional institutions
As of April 3, 2020, the most recent survey data cover approximately 320 correctional facilities in 47 states. These facilities represent more than 267,000 inmates and 53,000 correctional and health care staff.
The data are primarily drawn from jails (70%), with prisons accounting for 20% and other detention facilities, such as juvenile facilities, making up the remainder of the sample. These data may not be fully representative of all correctional institutions.
“This is a truly innovative public health effort,” says Brent Gibson, MD, MPH, chief health officer at NCCHC. “It underscores that there is no bright line between correctional health care and community health. The work we are doing now not only brings immediate understanding and perspective, but also will fuel studies and programs for years to come. The lessons learned here will be beneficial far into the future.”
The collaboration will continue to collect data on the pandemic’s effect on correctional facilities, as well as other correctional health care topics, in the months ahead. Information and reports are posted at https://www.ncchc.org/study-of-covid-19-in-correctional-facilities. The researchers urge all facilities to participate.
Findings to Date
Between March 25 (the initial survey) and April 3 (the latest daily follow-up), the number of reported COVID-19 cases among participating correctional facilities increased steadily (see Figure 1). The highest number of reported cases was among correctional staff—including health care staff and correctional officers. Specifically, the number of COVID-19 cases among staff increased from 136 to 245 among approximately 100 facilities that have consistently reported on a daily basis. During this period, the number of cases among inmates increased from 32 to 67 among approximately 100 facilities that consistently reported. In addition, there were two reported deaths among correctional staff.
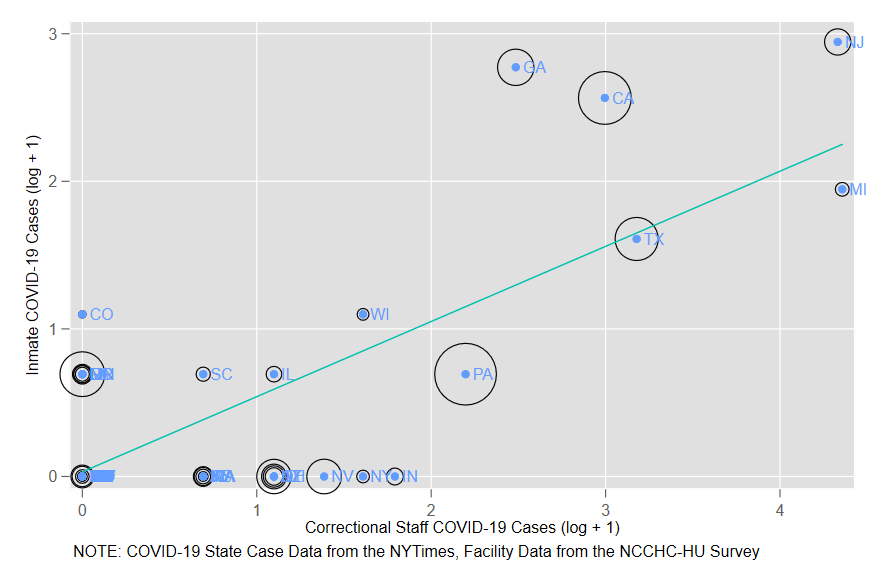
Combining the survey data with COVID-19 case data from the New York Times, the reported cases among correctional staff are highly correlated with cases in the broader community (see Figure 2). States that have been especially hard hit by the pandemic, such as Michigan and New Jersey, are also locations where correctional officers are more affected. At the state level, reported correctional staff cases are also correlated with reported cases among inmates (see Figure 3).
As of April 3, approximately two-thirds of participating facilities reported having adequate personal protective equipment (PPE) for their staff. Approximately 60 percent reported having access to laboratory testing for COVID-19. However, in the comments section of the survey, several facilities reported struggling to obtain adequate PPE and testing. They also noted long waits to receive test results, leading to uncertainty as to how to handle individuals who might be in jail for only a short time.
Exhibits
Figure 1: Cumulative Cases of COVID-19 Among Staff and Inmates
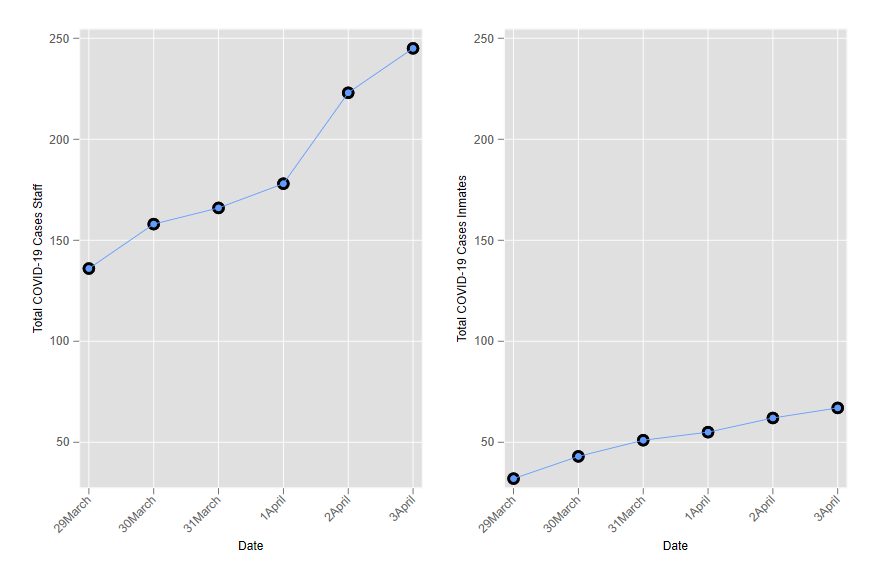
Figure 2: Correlation Between COVID-19 Infections in Staff and Community
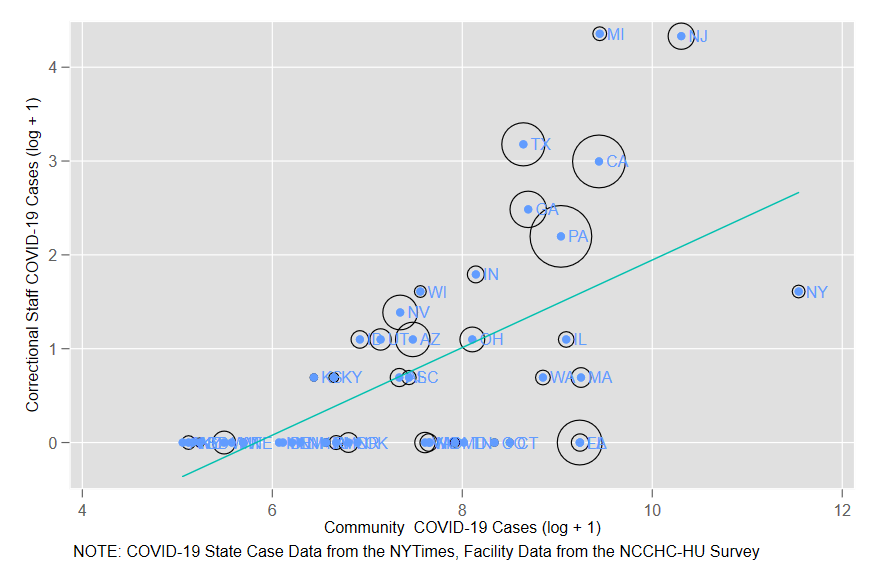
Figure 3: Correlation Between COVID-19 Infections in Inmates and Staff
About the National Commission on Correctional Health Care

The mission of the National Commission on Correctional Health Care, a nonprofit 501(c)(3) organization, is to improve the quality of health care in jails, prisons and juvenile confinement facilities. NCCHC establishes standards for health services in correctional facilities, operates a voluntary accreditation program for institutions that meet those standards, produces and disseminates resource publications, conducts educational conferences and offers a certification program for correctional health professionals. NCCHC is supported by the major national organizations representing the fields of health, mental health, law and corrections. Each of those supporting organizations has named a liaison to the NCCHC board of directors to create a robust, multidisciplinary governing structure that reflects the complexities of correctional health care.
About the Harvard University Researchers

Marcella Alsan is a Professor of Public Policy at Harvard Kennedy School. Alsan received a BA from Harvard University, a master’s in public health from Harvard School of Public Health, an MD from Loyola University, and a PhD in Economics from Harvard University. Alsan trained at Brigham and Women’s Hospital Hiatt Global Health Equity Residency Fellowship, then combined her PhD with an Infectious Disease Fellowship at Massachusetts General Hospital.
Crystal S. Yang is a Professor of Law at Harvard Law School. Yang received a BA in Economics, MA in Statistics, and PhD in Economics from Harvard University, and a JD from Harvard Law School. Yang previously worked as a Special Assistant United States Attorney in the U.S. Attorney’s Office for the District of Massachusetts.